Stopping depressive relapse is a serious aim within the administration of bipolar dysfunction. It has been proven that despair makes up round 72% of total time spent in poor health in folks with bipolar (Forte et al., 2015), and that bipolar despair particularly is related to vital bodily and psychological morbidity, in addition to elevated mortality (Baldessarini et al., 2020).
Lithium is the first-line really useful remedy for stopping bipolar despair (NICE, 2014). Nevertheless, as a earlier Elf weblog has highlighted, prescription of lithium is declining, each within the UK and different international locations (Edward, 2019). Antipsychotics, different temper stabilisers and – though not really useful by NICE – antidepressants are additionally typically prescribed long-term for folks with bipolar dysfunction. As just lately blogged right here and right here, the usage of antidepressants within the long-term administration of bipolar dysfunction is controversial, with the danger of temper destabilisation related to antidepressant monotherapy, and it is strongly recommended that they need to be prescribed for sufferers with bipolar dysfunction solely in particular scientific eventualities (McIntyre et al., 2020; Pacchiarotti et al., 2013).
In a paper just lately revealed in The Lancet Psychiatry, Ermis et al (2025) aimed to check whether or not the prescription of medicines utilized in bipolar despair have an effect on the possibilities of sufferers with bipolar dysfunction being admitted to hospital because of a depressive temper episode.

Stopping depressive relapse is a serious aim within the administration of bipolar dysfunction.
Strategies
Ermis et al used a cohort examine design to determine whether or not prescription of temper stabilisers, antidepressants and antipsychotics (prescribed and allotted) have been related to admission to hospital as a result of depressive sickness (main consequence), and admission to hospital as a result of mania or a somatic situation (secondary outcomes). Topics and consequence information have been recognized from ICD-10 codes (WHO, 2019) in Swedish nationwide registers from 2006-2021, while information on topics’ drugs have been gathered from the Prescribed Medicine Register.
A within-subjects Cox regression evaluation (adjusted for time-variant covariates similar to time since cohort entry and use of different psychopharmacological drugs) was used to check intervals of time during which the topic was prescribed a selected remedy towards instances during which no antidepressant, antipsychotic, or temper stabiliser have been prescribed. A lot of sensitivity analyses have been additionally carried out, to make sure the robustness of the findings.
Outcomes
105,495 folks with bipolar dysfunction have been included. The imply age of the pattern was 44.2 years (commonplace deviation, SD 18.8), and 62.2% of the pattern recognized as girls. Comorbidities have been current in a big minority (nervousness issues 40.5%, substance use dysfunction 18.8%, character issues 10.4% and former suicide try 10.6%).
Comply with-up was commenced from the date of bipolar analysis and the imply follow-up time was 9.1 years (SD 5.1). At follow-up, antidepressant monotherapy was the most typical publicity (utilized by 59,963 topics, 56.8% of the cohort, sooner or later in the course of the follow-up interval), adopted by temper stabiliser monotherapy (47,931, 45.4%) and antidepressant-mood stabiliser mixture (46,318, 43.9%).
General, 16,190 topics (15.3%) have been hospitalised with a depressive episode no less than as soon as in the course of the follow-up interval; 8,066 topics (7.7%) have been hospitalised as a result of mania.
Decreased likelihood of depression-related hospitalisation
Temper stabiliser monotherapy was the one remedy group discovered to be related to a decreased likelihood of depression-related hospitalisation in contrast with the prescription of no drugs in any respect (adjusted hazards ration, aHR 0.89, 95% confidence interval, CI 0.81 to 0.98).
Temper stabilisers mixed with antipsychotics have been related to a slightly decreased likelihood of depression-related hospitalisation, however this was not statistically vital (aHR 0.92, 95% CI 0.85 to 1.00).
In particular person remedy evaluation, solely lithium was related to a decreased likelihood of admission as a result of despair on this cohort of individuals with bipolar dysfunction (aHR 0.75, 95% CI 0.67 to 0.85).
Elevated likelihood of depression-related hospitalisation
Aside from temper stabiliser monotherapy and temper stabilisers mixed with antipsychotics, all different remedy teams, both alone or together, have been discovered to be related to an elevated likelihood of depression-related hospitalisation.
Notably, a number of drugs have been related to an elevated likelihood depression-related hospitalisation, specifically quetiapine, duloxetine, citalopram, olanzapine, mirtazapine, vortioxetine and aripiprazole.
Decreased likelihood of hospitalisation as a result of a somatic situation
When it comes to secondary outcomes, lithium was the one remedy related to a decreased likelihood of hospitalisation as a result of a somatic situation (aHR 0.86, 95% CI 0.80 to 0.93), with no statistically vital associations being discovered between the opposite drugs and somatic hospitalisation.
Elevated likelihood of mania-related hospitalisation
Antidepressants-only have been the one group that have been related to elevated possibilities of hospitalisation as a result of mania (aHR 1.22, 95% CI 1.03 to 1.44); all different drugs teams, alone or together, have been related to decreased possibilities of mania-related hospitalisation.
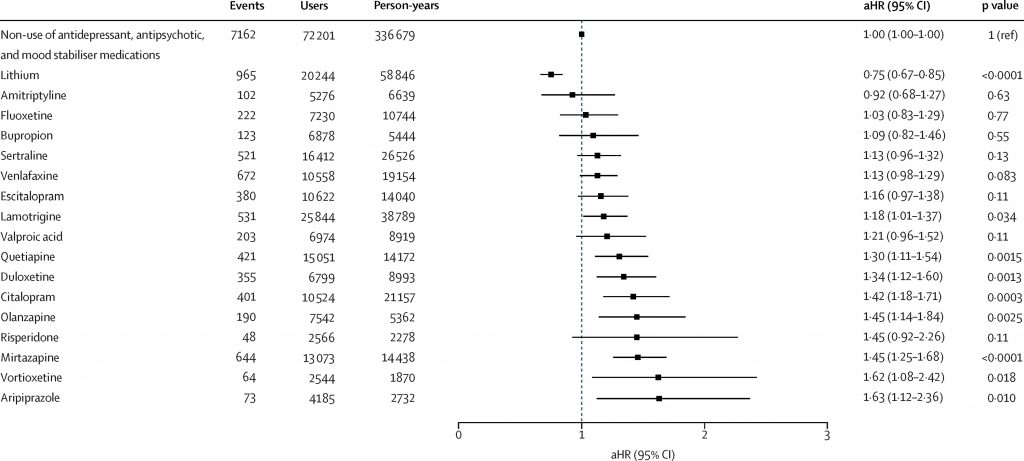
In particular person remedy evaluation, solely lithium confirmed a decreased likelihood of depression-related hospitalisation; all different drugs have been both equivocal or related to elevated likelihood of depression-related hospitalisation. [View full sized graphic]
Conclusions
The outcomes of this examine spotlight that lithium is the one monotherapy that decreases the possibilities of depression-related hospitalisation in folks with bipolar dysfunction. Further advantages have been additionally seen within the possibilities of mania-related and somatic hospitalisations, emphasising lithium’s multimodal advantages.
In distinction, sure antidepressants and antipsychotics have been related to elevated likelihood of depression-related hospitalisation.

“Present findings supported the notion that lithium ought to stay the mainstay of remedy in bipolar dysfunction” – Ermis et al, 2025
Strengths and limitations
A cohort examine design was the precise technique to reply this query. Cohort research, of their observational nature, permit researchers to determine the impact of exposures in pure environments, making the outcomes extra generalisable to real-life conditions. It additionally allowed the authors to check a number of drugs on the similar time, which might not have been potential to the identical extent in, for instance, an RCT design.
The examine inhabitants was taken from Swedish nationwide registers and ICD-10 codes have been used to establish these with bipolar dysfunction and the outcomes of curiosity. The outcomes are due to this fact reliant on appropriate software of the ICD-10 standards at time of analysis and proper coding of analysis into the well being registers. Inside these limitations, the authors have been capable of pattern a lot of the inhabitants with a bipolar analysis and supply follow-up over a number of years.
When it comes to the pattern demographics, charges of psychiatric comorbidity and suicide try historical past have been excessive, however this echoes the broader bipolar inhabitants (as highlighted by a earlier Elf weblog) and improves the generalisability of the outcomes from this pattern to real-world scientific settings. It’s notable, nonetheless, that there have been twice as many ladies than males, which isn’t reflective of bipolar dysfunction’s 1:1 male-to-female distribution and that information on ethnicity weren’t out there, each of which restrict the generalisability of the examine outcomes to specific teams.
The authors famous that by specializing in hospitalisation, the outcomes of this examine are solely related for probably the most extreme circumstances of bipolar despair and don’t think about the advantages or harms that these drugs could also be exerting in sufferers who’re managed totally as outpatients. Hospitalisation is an goal, binary measure that has vital real-world implications for sufferers, and so it may be argued that it’s nonetheless an excellent measure of the efficacy of those drugs.
A ultimate vital consideration is that use of registry information doesn’t all the time correspond precisely to behavior. In different phrases, simply because a prescription was written, doesn’t imply the remedy was taken. Usually talking, nonetheless, it’s possible that almost all of these prescribed a medicine do take it, and the massive numbers included on this pattern are prone to minimise the impact that remedy non-compliance in small minority might have on total outcomes.

Regardless of limitations, the massive pattern measurement and lengthy follow-up make the outcomes pretty generalisable to the bipolar inhabitants and vital scientific eventualities.
Implications for observe
This paper reaffirms the standing of lithium as “the best long-term remedy for bipolar dysfunction” (NICE, 2014). As such, it’s regarding that the charges of lithium prescription look like declining (Lyall et al., 2019). The explanations for this are unclear, however, as a earlier Elf weblog highlights, it could possibly be as a result of nervousness amongst sufferers and clinicians concerning the elevated monitoring that’s required for lithium or as a result of its particular hostile impact profile. It might even be associated to the low price of lithium, which can be driving the pharmaceutical business to promote the usage of various, dearer choices, doubtlessly swaying affected person desire. Regardless of the cause, a transfer away from prescribing lithium poses the danger of many sufferers lacking out on its potential advantages.
After lithium, the second- and third-line NICE-recommended preventative drugs for bipolar dysfunction are antipsychotic monotherapy and augmentation with valproate. This paper confirmed that these drugs have been related to reductions in mania-related hospitalisation, however no such profit was seen with depression-related hospitalisation. Some antipsychotics have been in reality related to elevated likelihood hospitalisation as a result of a depressive episode. This will make clinicians suppose twice about prescribing antipsychotics or valproate long-term in bipolar dysfunction if the first purpose of remedy is to forestall additional depressive relatively than manic relapses. In lots of sufferers this would be the purpose, notably as despair makes up nearly all of sickness time in these with bipolar dysfunction (Forte et al., 2015).
So, on the very least, Ermis et al have demonstrated the necessity for additional analysis on this space in order that we are able to make clear whether or not present scientific pointers for prevention of bipolar relapse are match for objective for every type of temper episodes, particularly in these for whom lithium isn’t an choice.

A transfer away from prescribing lithium poses the danger of many sufferers lacking out on its potential advantages.
Assertion of pursuits
No conflicts of curiosity to declare.
I’m presently in receipt of PhD fellowship funding by a Wellcome Belief-funded examine in bipolar dysfunction, sleep and circadian rhythm (www.ambientbd.com).
Hyperlinks
Major paper
Ermis, C., Taipale, H., Tanskanen, A., Vieta, E., Correll, C. U., Mittendorfer-Rutz, E., & Tiihonen, J. (2025). Actual-world effectiveness of pharmacological upkeep remedy of bipolar despair: a within-subject evaluation in a Swedish nationwide cohort. The Lancet Psychiatry.
Different references
Alsaif, M. (2017). Antidepressants for bipolar despair. Nationwide Elf Service.
Baldessarini, R. J., Vázquez, G. H., & Tondo, L. (2020). Bipolar despair: a serious unsolved problem. Worldwide journal of bipolar issues, 8(1), 1.
Edward, D., & Ahmed, S. (2019, 14 June 2019). Prescribing lithium for bipolar dysfunction: are we too scared? The Psychological Elf.
Forte, A., Baldessarini, R. J., Tondo, L., Vázquez, G. H., Pompili, M., & Girardi, P. (2015). Lengthy-term morbidity in bipolar-I, bipolar-II, and unipolar main depressive issues. J Have an effect on Disord, 178, 71-78.
Kalfas, M. & Leeks, P. (2024). Jury stays out on antidepressant-induced mania. Nationwide Elf Service.
Lyall, L. M., Penades, N., & Smith, D. J. (2019). Modifications in prescribing for bipolar dysfunction between 2009 and 2016: national-level information linkage examine in Scotland. The British Journal of Psychiatry, 215(1), 415-421.
McIntyre, R. S., Berk, M., Brietzke, E., Goldstein, B. I., López-Jaramillo, C., Kessing, L. V., Malhi, G. S., Nierenberg, A. A., Rosenblat, J. D., & Majeed, A. (2020). Bipolar issues. The Lancet, 396(10265), 1841-1856.
NICE. (2014). Suggestions | Bipolar dysfunction: Evaluation and Administration | Steering | NICE. Nationwide Institute for Well being and Care Excellence.
Pacchiarotti, I., Bond, D. J., Baldessarini, R. J., Nolen, W. A., Grunze, H., Licht, R. W., Put up, R. M., Berk, M., Goodwin, G. M., & Sachs, G. S. (2013). The Worldwide Society for Bipolar Issues (ISBD) activity pressure report on antidepressant use in bipolar issues. American Journal of Psychiatry, 170(11), 1249-1262.
Pell, C. (2013). Summing up suicide information in bipolar dysfunction. The Psychological Elf.
WHO. (2019). ICD-10 Model:2019. World Well being Organisation.
Picture credit
Source link



